Pain is a complex phenomenon that often stems from sources beyond simple muscle tension. In recent decades, healthcare practitioners have increasingly recognized the role of fascia—the connective tissue network that surrounds and penetrates muscles, organs, and other structures throughout the body—in creating chronic pain patterns. Understanding fascial restrictions and their treatment requires examining both the limitations of traditional approaches and the promises and challenges of newer therapeutic methods.
What Is Fascia?
Fascia is a continuous web of connective tissue composed primarily of collagen fibers, elastin, and a gel-like ground substance. This tissue forms a three-dimensional network throughout the body, connecting everything from the surface of the skin to the deepest organs. Rather than existing as separate layers, fascia forms an interconnected system that transmits force, provides structural support, and plays a crucial role in movement and posture.
Recent research has revealed that fascia is far more than passive packaging material. It contains numerous sensory receptors, can contract independently, and plays an active role in proprioception (body awareness) and pain perception. This understanding has revolutionized how we think about chronic pain and movement dysfunction.
How Fascial Restrictions Develop
Fascial restrictions occur when the normally fluid and adaptable fascial tissue becomes dense, dehydrated, or adhered. Several factors contribute to these changes:
Physical Trauma: Injuries, surgeries, and repetitive strain can cause fascial tissue to thicken and lose elasticity as part of the healing process. While this protective response helps stabilize injured areas, it can create long-term movement restrictions.
Postural Habits: Prolonged positioning, whether from desk work, driving, or other activities, can cause fascia to adapt to shortened or lengthened positions, creating imbalances throughout the body’s tensional network.
Emotional and Psychological Stress: Research suggests that emotional stress can manifest as physical tension in fascial tissue, potentially creating or maintaining pain patterns long after the initial stressor has passed.
Inflammation and Dehydration: Systemic inflammation and inadequate hydration can affect the gel-like ground substance of fascia, reducing its ability to glide smoothly and transmit force efficiently.
The Pain Pattern Puzzle
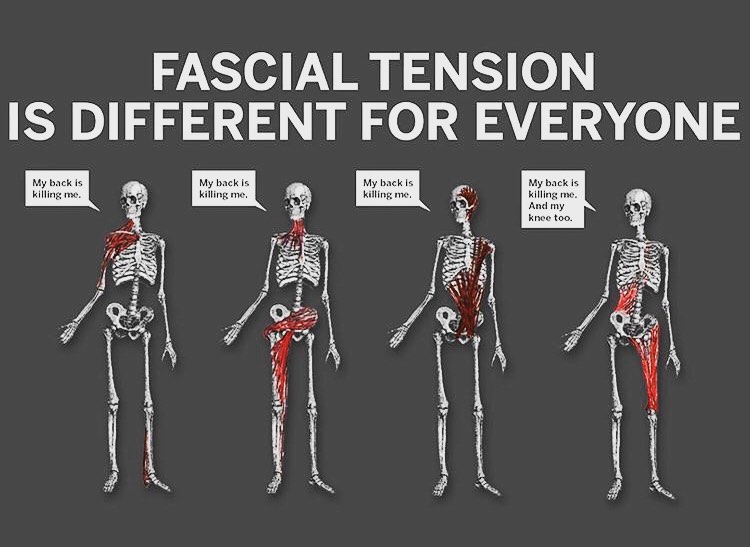
Fascial restrictions rarely cause pain only at their location. Because fascia forms a continuous network, restrictions in one area can create compensatory patterns throughout the body. For example, a restriction in the plantar fascia of the foot might contribute to knee pain, hip dysfunction, or even headaches as the body adapts its movement patterns to accommodate the limitation.
This interconnectedness explains why pain often appears in areas distant from the original problem and why treating only the painful area may provide temporary relief without addressing the underlying cause. The fascial system’s continuity means that effective treatment often requires a whole-body perspective rather than a localized approach.
Limitations of Traditional Massage
Traditional massage therapy, while beneficial for many conditions, faces several limitations when addressing fascial restrictions:
Depth and Duration: Fascial restrictions often exist in deeper layers that standard massage techniques may not adequately reach. Additionally, fascial tissue responds better to sustained pressure over time rather than the rhythmic movements typical of many massage styles.
Scope of Treatment: Traditional massage typically focuses on muscles and may not specifically address the fascial connections between different body regions. This can result in temporary relief without resolving the underlying fascial patterns creating the dysfunction.
Integration with Movement: While massage can help release tension, lasting change often requires integrating new movement patterns. Traditional massage, performed with the client passive on a table, may not provide opportunities to retrain movement habits.
Alternative Approaches and Their Tradeoffs
Several therapeutic approaches have emerged to address fascial restrictions more specifically:
Structural Integration (Rolfing): This approach uses slow, deep pressure to reorganize fascial layers and improve overall body alignment. While potentially effective for creating lasting change, it can be uncomfortable and requires a significant time and financial commitment (typically 10-12 sessions).
Myofascial Release: This technique applies sustained pressure to restricted areas, allowing the fascia to slowly release. It can be gentler than structural integration but may require numerous sessions to achieve lasting results. The challenge lies in accurately identifying all contributing restrictions.
Instrument-Assisted Soft Tissue Mobilization: Tools like Graston instruments or gua sha can help practitioners apply specific pressure to fascial restrictions. While these can be effective, they require skilled application to avoid tissue damage and may cause temporary discomfort and bruising.
Movement-Based Approaches: Methods like Feldenkrais, yoga therapy, or corrective exercise address fascial restrictions through movement re-education. These approaches can create lasting change but require active participation and consistent practice from the client.
The Challenge of Lasting Change
Creating permanent change in fascial patterns faces several obstacles:
Neurological Adaptation: The nervous system adapts to long-standing patterns, making them feel “normal” even when dysfunctional. Changing these patterns requires not just tissue release but nervous system re-education.
Lifestyle Factors: Unless the activities or postures that created the restrictions change, the patterns are likely to return. This requires clients to actively participate in their recovery through ergonomic changes, movement practices, or stress management.
Complexity of Patterns: Most people develop multiple, interconnected fascial restrictions over time. Addressing one area may reveal previously hidden restrictions elsewhere, making treatment an ongoing process rather than a quick fix.
Individual Variation: Each person’s fascial system is unique, influenced by genetics, injury history, activity levels, and numerous other factors. What works well for one person may be ineffective or even counterproductive for another.
Finding Balance: An Integrated Approach
Given the complexity of fascial restrictions and their role in pain, the most effective approach often combines multiple strategies:
Assessment First: Comprehensive evaluation to identify not just areas of pain but patterns of restriction throughout the body helps create a targeted treatment plan.
Combining Modalities: Using manual therapy to release restrictions while simultaneously incorporating movement re-education and strengthening can address both the tissue changes and the movement patterns that created them.
Patient Education: Understanding how daily activities affect fascial health empowers individuals to make choices that support long-term improvement rather than perpetuating dysfunction.
Realistic Expectations: Acknowledging that fascial change takes time—often weeks to months—helps set appropriate goals and prevents disappointment with the pace of progress.
Conclusion
Fascial restrictions represent a significant but often overlooked contributor to chronic pain patterns. While traditional massage therapy provides valuable benefits, addressing fascial dysfunction typically requires more specific approaches that consider the interconnected nature of the fascial system and the need for active participation in the healing process.
The key to lasting change lies not in any single treatment modality but in understanding the unique patterns each individual has developed and creating a comprehensive approach that addresses both the physical restrictions and the habits that created them. As our understanding of fascia continues to evolve, so too will our ability to effectively treat the complex pain patterns it can create.
By recognizing both the potential and limitations of various treatment approaches, individuals and practitioners can work together to develop strategies that provide not just temporary relief but lasting improvement in function and quality of life.